The World Health Summit is an annual global health policy conference that was held this year in Berlin on October 27-29. Addressing a global theme of “The Impact of Climate Change on Health”, the Summit brought together key stakeholders from academia, policymaking, industry, international organisations, and civil society representing more than 100 countries.
Governance Post Executive Editor Mahima Shah Verma spoke with Bernado Mariano, Chief Information Officer of the WHO, and Ali Jafarian, President of the 2019 WHS Summit and world-renowned liver transplant surgeon. Mariano talked about his experiences managing rapid advancements in technology while balancing data security and ethical practices. Jafarian reflected on the decades-long evolution of Iran’s medical system following the establishment of the Islamic Republic. He spoke to the challenges of incorporating new technologies given economic constraints, his motivations in becoming a surgeon, the impacts of war on mental health, and how Iran provides free liver transplant surgeries to all its citizens.
Bernardo Mariano Júnior is the Chief Information Officer of the World Health Organisation. Before his leadership position at the WHO, Mariano worked extensively in the fields of information management, communication, and partnerships as CIO, Director of Communications and Technology, and Senior Regional Adviser for the International Organisation for Migration (IOM) based in Sub Saharan Africa and South Africa, respectively.
The Governance Post: How do you approach the management of the WHO’s health data and services in a digital ecosystem?
Bernardo Mariano: As the WHO, we must first make our products, services, and processes available in the digital ecosystem. We must rethink access to the guidelines and recommendations we produce, such as the pre-qualifications of vaccines and medications: How will these look in the digital ecosystem – as tablature? Until very recently, we were producing this for ministries of health, hospitals, and practitioners, but in the digital ecosystem, it all goes straight to the end-user. How can we impact the individual if we are only talking to policymakers, and the market is talking to the consumers? Take, for example, the anti-vaccine movement. We end up with the resurgence of measles, a disease that had been eradicated in many countries, including in the US and Europe.
GP: Where does one draw the line of ethics and transparency between data protection and data collection for scientific research and industry application?
BM: The WHO believes that platforms have the responsibility to direct users to accurate information. How do we globally govern data? Should we have a bill of rights to protect private health data from being monetized? Some participants at the World Health Summit approached me saying: “If a platform is using my health data for monetization, then I should receive a share of that revenue!” I think this is a valid claim. On the other hand, we need to collect large volumes of de-personalised data for research on health impacts. This requires access to and free flow of data. These are the two sides that we need to balance. One cannot stifle the other. We must not create unintended consequences. The private sector’s responsibility is another issue.
GP: Thank you very much.
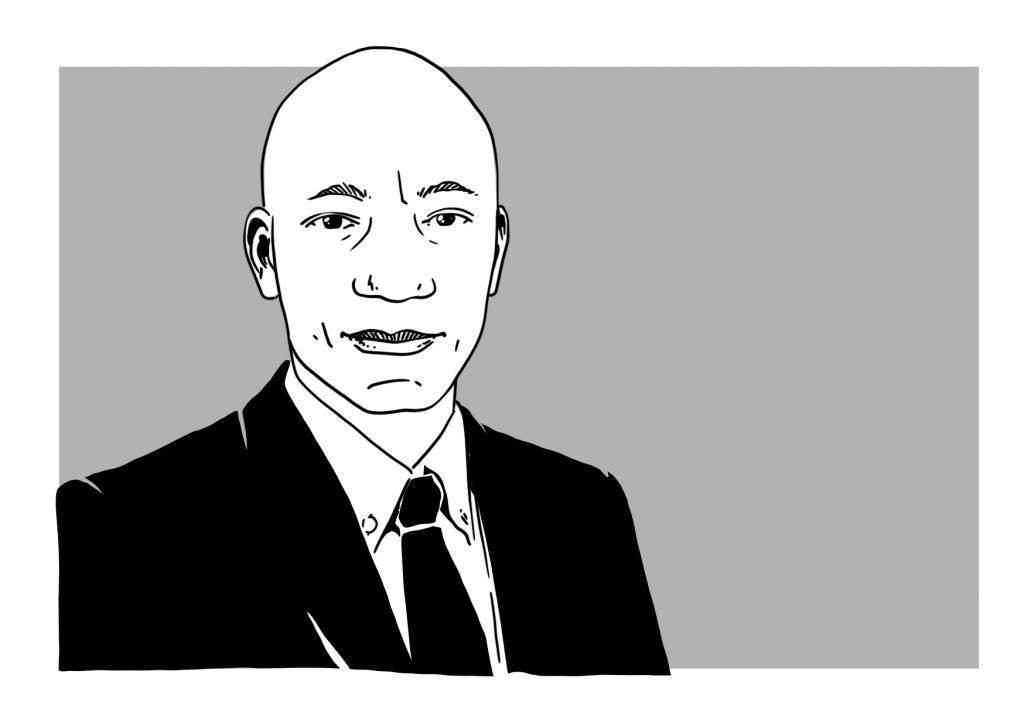
Ali Jafarian M.D. is the 2019 International President of the World Health Summit. He is the Founding Chief of the Division of Hepatobiliary & Liver Transplantation at the Imam Khomeini Hospital in Tehran, Iran. He is a distinguished Professor at the Department of General Surgery at the School of Medicine and Member of the Board of Trustees at the Tehran University of Medical Sciences (TUMS).
GP: What are the key consequences of the recent advancements of technology in medical practice? How have your professional experiences in Iran informed your understanding of the uses and limitations of technology in healthcare?
Ali Jafarian: In the past four decades, we have been advancing very swiftly in imaging technologies and electronic health records for general populations in easily accessible digitalised bases. Technology is a very good instrument in public healthcare for having, transferring, and applying population data for research. In Iran, we have a national plan to integrate everybody’s basic data in a health system, more specifically, through a detection plan for hypertension. In this way, we can increasingly control the occurrence of non-communicable diseases, which are one of the main causes of premature death. In some specialties, we are dependent on instrumental technologies, such as imaging and operating rooms. Of course, there is not an even distribution of technology around the world, across regions and generations. When a new technology is first introduced, it is usually very expensive. Over time, even though these expenses decrease, they can be patented, so many parts of the world lack access. In Iran, we have limited availability of affordable health technologies, which means we must cope accordingly. As a whole, I believe Iran is doing well technology-wise. Due to the sanctions, we have difficulties repairing instruments and getting parts, more so with acquiring new instruments altogether; however, we are working hard to cover these deficits. The incubators are making technological growth possible, but there is no rationale to make everything by ourselves. There are only few countries in the world, if any, that are totally independent with regards to technology. One or two of the best Iranian incubators are focused on medical equipment and medicines. They are making instruments and machines that are needed, but not all are in clinical use. There are not many companies making CT scanners in Iran and many other countries, so we need to import them from major producers including Siemens, Phillips, and GE. Making these types of technologies requires large initial investments and a market for them. Without a market, it’s not cost-effective for investment.
GP: You have worked extensively in the field of organ transplants in Iran. What role do ethics play in the allocation liver transplants and related services that you and your teams provide?
AJ: My main job is in liver transplants at the Imam Khomeini Hospital Complex, a big tertiary care hospital complex in Tehran. Everybody has access to liver transplants, which are free of charge in Iran for the patient from the time of admission until discharge. Only the preoperative workups and post-operative treatments and drugs are co-paid by the patient and insurance. The Ministry of Health covers the liver transplant costs, due to a major decision made in Iran 35 years ago due to a huge need. Social Insurance could not cover it, so we had to send people abroad for kidney and liver transplants at very high expenses. For liver transplants, we base our decisions on scientific and medical criteria. We plan and work ethically because we give higher priority to the recipient based on the severity of their condition. A scoring system that prioritises patients with end-stage liver disease is the main criterion to enter the transplant list. Most of our organs are from brain-dead donors; we do not have any organ-selling of livers nor do we conduct liver transplants from unrelated living donors. I think ours is a good, ethical backbone for this treatment. In the 18 years that I have been doing liver transplants, we have not encountered major problems and have established this practice countrywide. We currently have two high volume centres that are performing at least 150 transplants a year and five smaller centres that are in the beginning stages. There is no one body that has told the others to do it, rather it is a consensus among the liver transplantation centres.
GP: Is it a physician’s responsibility to provide education concerning prevention for liver disease? How do you share information about access to medical services and treatments in Iran?
AJ: Whenever I have an opportunity, I talk to people on TV and in the media. We communicate the number of people who need liver transplants resulting from fatty liver disease using Iranian and international media like Telegram and Whatsapp. In Iran, the danger of fatty liver is a well-known issue. Yet, nobody is putting aside the pizzas and burgers. I think this is a question of the ethics of social media. I think it is unethical for people to post whatever they like without evidence. This kind of openness is a major problem. I’m not saying we should censor data, but I do think we need digital literacy.
GP: How do you define good health and how an individual achieves it? Do you have any life, professional, or academic experiences that have informed your perspectives on what health is?
AJ: You can look at human beings as bio-psycho-social-spiritual units. Here we have four dimensions: “Bio” is what we usually talk about in terms of primary, secondary, or tertiary healthcare; “Psycho” is when we refer to mental health and related issues; Social health is really related to society and its governance and varies across countries due to cultural differences. Spiritual health is completely different. This is why a lot of people feel as if something is lacking even if they are physically and psychologically fine. This kind of health is difficult both to define and achieve. Some people turn to religion, while others don’t even know that spiritual health even exists – that the soul of the human is real and must be tended to. In healthcare, we usually deal with bio and psycho. Social health is, to a great extent, out of our reach. Society is not healthy in many parts of the world, even if the people themselves are. Conversely, when society is not healthy, people are affected too.
GP: What were your motivations for becoming a surgeon?
AJ: I’m not sure exactly why, but I decided to go into surgery at the age of 12. A family member was living in the US who was a pediatrician and allergist. I used to meet him once a year when he came back to Iran. At the time, about 45 years ago when I was in elementary school, there were no allergy specialists in Iran. So when he visited, he gave medication to everybody with allergy problems. I found it amazing how he helped others.
GP: Who in the Iranian community is responsible for caregiving, and how does this impact medical practice and administration?
AJ: In the West, the family is less important after the age of 18. In the East, this is not the case: family is always family – at least in most parts. With industrialisation, more Western ideas have caused disruption, but family is still significant and holds the responsibility to support other members. So this is both spiritual and cultural. Fortunately in Iran, the family structure is still strong, so for any problem, not just psychiatric or psychological, the family usually provides support. Usually, a lot of family members are around a patient when they are admitted and we have to explain everything to them
GP: How has medical education in Iran developed in response to the digitalisation of health and the need for digital literacy in the training of doctors?
AJ: Iran has advanced astonishingly well in medical education over the last four decades, increasing the number of its medical practitioners five-fold. We were sending patients abroad for many disease treatments in the 70s and 80s, and now this is completely unnecessary. Before the 1979 Iranian Revolution, we had many foreign physicians in Iran especially from India, Bangladesh, and Pakistan – both general practitioners and specialists. After the Revolution, there were no more expatriate physicians in Iran within 10 years. The government decided to integrate medical education and health services and use health service facilities for medical education, such as adding to the list of teaching hospitals. In this way, Iran was able to significantly increase the number of medical students. Higher education in Iran is divided into two types of universities that are structurally separate: a comprehensive type administered by the Ministry of Education and universities of medical sciences administered by the Ministry of Health and Medical Education. This decision for structural separation was made 35 years ago because we lacked an adequate number of health providers. Although we still lack physicians in Iran, the shortage is smaller. I think we are training sufficient numbers of physicians now. The main issue is how we can get those jobs. How can we compensate for them coming to work in the system?
GP: Around a quarter of people in Iran are reported to suffer from mental illness. What are the challenges for access to and quality of services for mental healthcare in Iran?
AJ: If you compare the region (West Asia and North Africa) with the rest of the world, you will find a greater number of people suffering from mental health conditions, because it is an inflamed region. There are always tensions and conflict, especially in the form of wars. Good data would show a large proportion of people with mental health issues, including major depression and anxiety disorders. These people need help. At TUMS, there has already been a seven-year plan for community mental health centres (CMHCs) introduced in 2012. These CMHCs go to communities and educate general practitioners to locate and identify psychiatric needs. My colleagues have been working in the southern part of Tehran, which is in the territory of TUMS and the area that we cover for primary healthcare. They started a similar programme around the country five or six years ago to achieve universal health coverage. There is a hierarchy from health houses in the villages up to the health centres in the cities, including secondary and tertiary hospitals. In comprehensive health centres, there are psychologists in the teams to deal with these issues. Mental health is a universal problem. Going into depth in mental healthcare is, of course, a specialisation. For medical students in Iran, there is a rotation into psychiatric hospitals. This is why the CMHC programme is targeted at general practitioners, not psychiatrists because there just aren’t enough psychiatrists to cover 25% of the population. The CMHC programme educates GPs about minor depression or anxiety disorders so that they can find these cases and help to control them. Mental health is part of medical education like other disciplines.
GP: What lessons about the efficient and ethical provision of healthcare can global health practitioners learn from Iran, especially in the field of liver transplants?
AJ: To have the best quality of medical service, we need a lot of money; however, everybody in Iran has basic health services and 90% coverage of inpatient admissions. In places like Canada and the UK, it takes a long time for the system to provide basic health services. We achieved the provision of free liver transplants in Iran based on our potential. It has been hard work for 20 years, but it can be done. We are doing all kinds of difficult liver transplants in Iran in two major, globally renowned centres in Tehran and Shiraz. The latter is a very large centre that performed over 600 liver transplants in one year (2017). We are now performing 170-180 liver transplants per year. In the US, 144 services are providing this treatment. In terms of volume, our centre is competing with only three American centres and only two in the UK. Regarding the outcome, the long-term survival of our patients after liver transplants is now 78-80% ( Arch Iran Med. July 2018;21(7):275-282), which is comparable with the average in the US, with just 3% of the costs. Iran cannot afford to spend 18% of its GDP on health and remain at about number 50 globally on health indicators. We must manage everything much more economically to match our resources. This is why I am so honoured that we have done one thousand liver transplants without taking a single penny from the patients.
GP: Thank you very much.
This interview has been edited and condensed for readership.


Mahima Shah Verma is the Editor of the Governance Post and a candidate for the Masters of International Affairs at the Hertie School. She has a B.A. in History from the University of Southern California, specialising in oral history and photojournalism of mass violence and genocide in Europe and Central and South Asia during the 20th century. She is passionate about writing, singing, photography, and learning languages. Her ongoing research is in international and humanitarian law, armed conflict, peacekeeping, and social policy.